Getting to the Root of Visceral Pain

Getting to the Root of Visceral Pain
February 24, 2024Researchers at MSU may have discovered why visceral pain is so common in people who have experienced inflammation in their guts, including patients with irritable bowel syndrome.
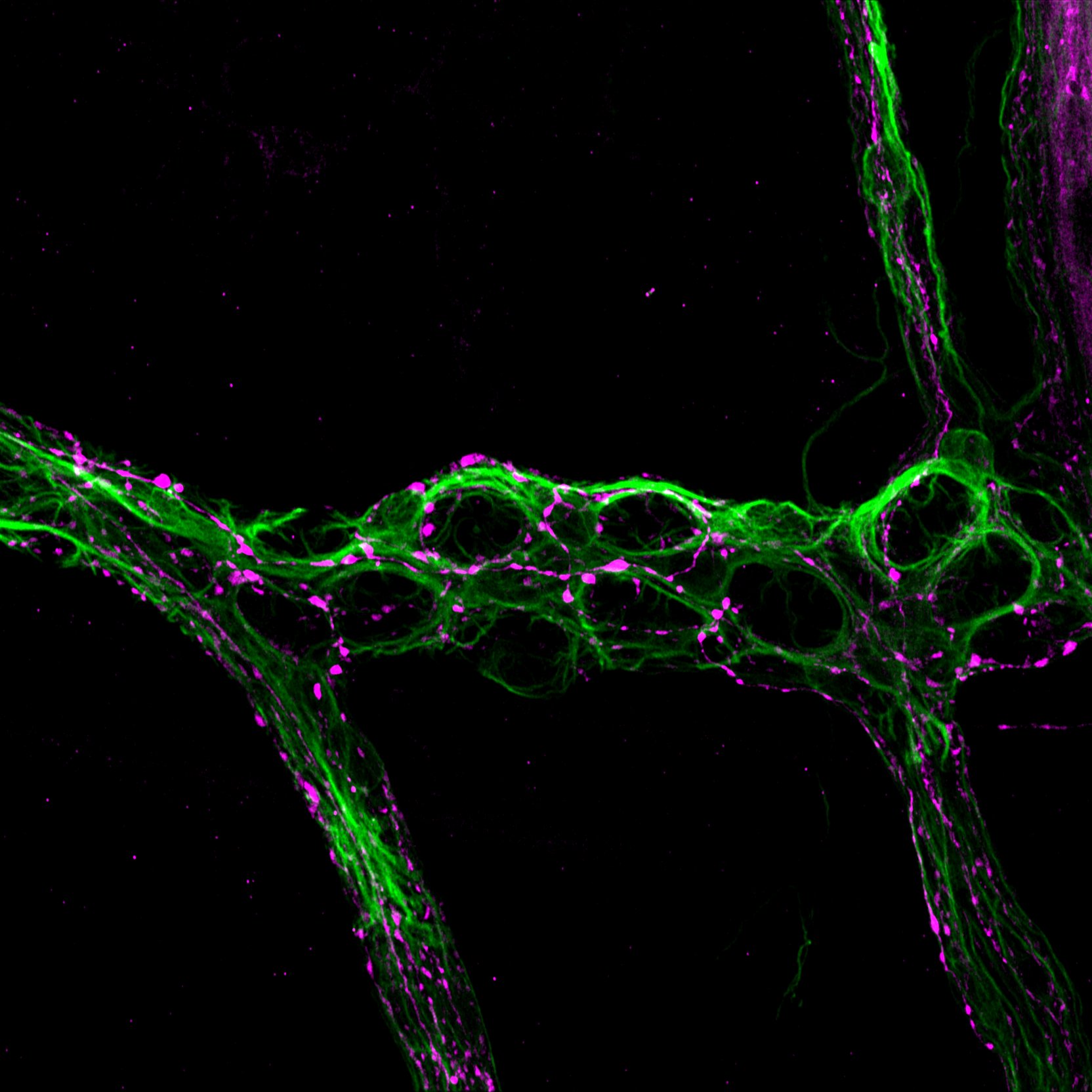
Working with mouse models, MSU physiologists showed that nervous system cells known as glia can sensitize nearby neurons, causing them to send pain signals more easily than they did prior to inflammation.
“The glia drop the threshold for activating a neuron,” said MSU Research Foundation Professor Brian Gulbransen, whose team’s new report was published in the journal Science Signaling. “So, something that wasn’t painful is now painful. It’s like when you put on a shirt after getting a sunburn.”
This discovery could help researchers develop therapies to lessen or eliminate visceral pain by counteracting the glia’s sensitizing efforts. Currently, no medicines on the market are designed to act directly on glia, but pharmaceutical companies are investigating that approach, Gulbransen said.
The investigation was spearheaded by Wilmarie Morales-Soto who earned her doctorate in 2023 working on this project in Gulbransen’s lab. She’s now a postdoctoral research fellow at the Mayo Clinic. The research team also included research associate Jacques Gonzales and William Jackson, a professor in the Department of Pharmacology and Toxicology.
Moving forward, Gulbransen and his team are eager to explore looming questions related to visceral pain.
For example, data show that females are more likely to experience visceral pain than males. Early life adversity, including stress and trauma, can also make people more susceptible to visceral pain.
Glia are implicated in both situations and learning more about them could help innovate new ways to treat gut pain.
Contributing Writer(s): Matt Davenport




